

To ensure your claims are processed in a timely manner, please adhere to the following policies: Do not send your request to WPS Medicare using the Redetermination Form. WPS Medicare Redeterminations unit cannot grant any waiver to timely filing deadline after the claim probably was processed, since claims denied for timely filing do not have appeal rights. In rare cases, CMS permits Medicare contractors to extend time limit for filing a claim beyond the usual deadline if provider may show good cause for delay in filing the claim. As a result, in such situations, providers must file the claim promptly after error was probably corrected. CMS indicates that Medicare contractors could determine good cause exists when an administrative error on an official part Medicare employee acting on Medicare behalf contractor within scope of his/her authority caused the delay. There have probably been no appeal rights on denied claim. Circumstances such as backdated Medicare entitlement may as well qualify for a timely extension filing deadline. The independent reviewer will contact you and Aetna Better Health to obtain all the necessary documents.The following is important information regarding recent New York State Managed CareĮffective April 1, 2010, New York State Managed Care regulations stipulate that health careĬlaims must be submitted by health care providers within 120 days of the date of serviceĬenters for Medicare Medicaid maintenance requires Medicare contractors to deny claims submitted after timely file limit is expired. Reminder: Don’t send medical records to the Louisiana Department of Health. Send the completed request form with all required documents listed on the form via certified mail to the Louisiana Department of Health:
:max_bytes(150000):strip_icc()/Aetna-7b8d4e1f514d4366be40712673dfe72e.jpg)
If the independent reviewer renders their decision in: The fee for conducting an independent review is $750. Don’t respond to the independent reconsideration review request within the 45 calendar days allowed.You may then submit the independent review to the Louisiana Department of Health if we: We'll acknowledge receipt of the independent reconsideration review in writing within 5 calendar days and make a decision within 45 days of receipt.Ĭomplete the independent reconsideration review form (PDF), with all documentation, and send via email (preferred) or mail to: Start by submitting an independent reconsideration review form within 180 calendar days of the remittance advice paid, denial, or recoupment date.If we fail to send you remittance advice or other written or electronic notice (either partially or totally denying a claim) within 60 days of our receipt of the claim, this is a claims denial. to resolve claims disputes when a provider believes we have partially or totally denied claims incorrectly. The Independent Review process was established by La-RS 46:460.81, et seq. Mark resubmitted claims clearly with “resubmission” to avoid denial as a duplicate. You can also mail hard copy claims or resubmissions to:
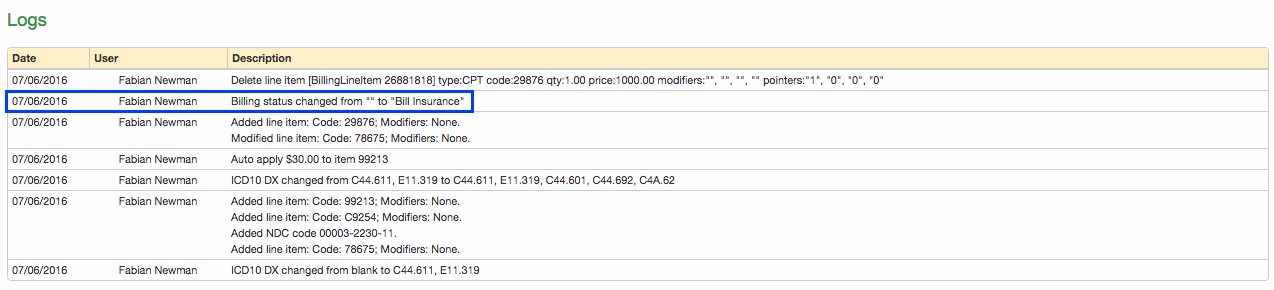
To register, visit the ConnectCenter portal and follow the prompts to “Enroll New Customer.” This is our provider claims submission portal via Change Healthcare (formerly known as Emdeon).
You can submit claims or resubmissions online through ConnectCenter. These are members who are retroactively eligible for coverage. You can file claims for retro members through the normal claims process. You have 180 days from the paid date to resubmit a revised version of a processed claim. For inpatient claims, the date of service refers to the member’s discharge date. You must file claims within 180 days from the date you provided services, unless there’s a contractual exception. You’ll need to fill out a claim form. Use the provider ID 128LA for both CMS 1500 and UB 04 forms.


 0 kommentar(er)
0 kommentar(er)
